
A deeper look at psoriasis pathogenesis: Watch the video to see the MOD in action
Psoriasis is a manifestation of an inflammatory cascade in response to stress or genetic triggers. These triggers correlate with increased infiltration of immune cells in the skin, including dendritic cells, T cells, and neutrophils.1
The activated keratinocyte powers an inflammatory feedback amplification loop
| Activated keratinocytes secrete cytokines and chemokines that perpetuate the inflammatory feedback amplification loop. IL-17C further activates Th17 cells and IL-36 stimulates dendritic cells.2-4 Chemokines, such as CCL20, IL8, and CXCL1, are secreted by activated keratinocytes to attract immune-mediating cells, which provide additional sources of IL-17A and IL-17F independent of IL-23, as well as proteases that activate IL-36.1,3,5 This persistent inflammatory feedback loop results in keratinocyte hyperproliferation and leads to the clinical symptoms of pain, itching, and skin plaques.1,3,6,7 |
Cytokines power the psoriasis inflammatory cascade
TNFα produced by dendritic cells and Th17 cells activates keratinocytes
TNFα was one of the first cytokines to be defined as pathogenic in psoriasis. TNFα is produced by various immune cells, including dendritic cells, and the keratinocytes themselves. It stimulates inflammation and hyperproliferation of keratinocytes in psoriatic lesions.1
IL-23 produced by dendritic cells moderates the T-cell pathway
IL-23 plays a key role in the T-cell pathway and is essential for the differentiation of Th17 cells.8
Internal or external triggers activate dendritic cells to produce IL-23. This is indicated by increased levels of the IL-23–characterizing p19 and p40 subunit mRNA in lesional skin compared with nonlesional skin (p19 and p40 mean increase of twenty twofold and twelvefold, respectively).9
The IL-23/17 interplay is known to be at the core of psoriasis immunopathology.3 Research shows that, as a result of IL-23 mediation, additional IL-17 subtypes become elevated in the skin. Importantly, IL-23 blockade does not completely inhibit IL-17 production, as other sources of IL-17 may be present.10
IL-23 is elevated in lesional vs nonlesional skin as measured by its subunits 9*
IL-23 produced by dendritic cells moderates the T-cell pathway
IL-23 plays a key role in the T-cell pathway and is essential for the differentiation of Th17 cells.8
Internal or external triggers activate dendritic cells to produce IL-23. This is indicated by increased levels of the IL-23–characterizing p19 and p40 subunit mRNA in lesional skin compared with nonlesional skin (p19 and p40 mean increase of 22-fold and 12-fold, respectively).9
The IL-23/17 interplay is known to be at the core of psoriasis immunopathology.3 Research shows that, as a result of IL-23 mediation, additional IL-17 subtypes become elevated in the skin. Importantly, IL-23 blockade does not completely inhibit IL-17 production, as other sources of IL-17 may be present.10
IL-23 is elevated in lesional vs nonlesional skin as measured by its subunits9*
IL-17A and IL-17F are produced by the innate and adaptive immune system
Th17 cells secrete IL-17A and IL-17F, both of which are present as homodimers and heterodimers and play critical overlapping roles in psoriasis pathogenesis.1
Most IL-17 family subtype cytokines are elevated in psoriasis. The abundance of IL-17F in psoriatic skin compared to nonlesional skin is more elevated than IL-17A. Both are important proinflammatory cytokines in the pathogenesis of psoriasis.1,11,12
The expression of Th17 cells both in circulation and in lesional skin has been shown to correlate clinically with the severity of psoriasis.1 IL-17A and IL-17F are produced by not only Th17 cells but also cells of the innate-like immune system, such as γδ T cells and ILC38,10
Varying IL-17 cytokine levels in psoriatic lesions12†
IL-17 cytokine fold increase in lesional vs nonlesional skin 11*
Th17 feedback amplification: IL-17C
Activated keratinocytes secrete IL-17C, which stimulates Th17 cells to propagate the cycle of inflammation in psoriasis. 2,13
IL-17C receptors are found on Th17 cells. This receptor is a dimer comprising IL-17RE and IL-17RA. In Th17 cells, IL-17RE gene expression was detected at a higher level than IL-23R, a receptor with known functional importance in these cells. Whereas IL-17RA is present in other receptor dimers, IL-17RE is unique to the IL-17C receptor; therefore, IL-17RE expression is a useful indicator of which cells are targeted by IL-17C.2,14
IL-17C is elevated in psoriatic skin, while its receptor is on Th17 cells
*Individuals with chronic plaque psoriasis provided biopsies (nonlesional and lesional) and protein expression was quantified by immunohistochemistry.
Dendritic cells feedback amplification: IL-36
IL-36 production by activated keratinocytes leads to further dendritic cell stimulation.3,4
In vitro assays of human cells have shown that IL-36α and IL-36γ are produced by keratinocytes
after stimulation with IL-17A, TNFα, and other proinflammatory mediators. Elevated levels of IL-36
cytokines can then activate dendritic cells, as evidenced by the presence of CD83 and CD86
markers.3,4
Stimulation with IL-17A elevates IL-36 production by NHEK cells 3*
IL-36 cytokines activate human dendritic cells 4†
Neutrophil feedback amplification chemokines (CXCL1, IL-8, and CCL20)
Activated keratinocytes in psoriatic lesions produce chemokines (e.g., CXCL1, IL-8, CCL20) that recruit neutrophils and other immune cells to the site of inflammation.1
These recruited neutrophils have the potential to secrete additional IL-17A and IL-17F that can further activate keratinocytes.5,10
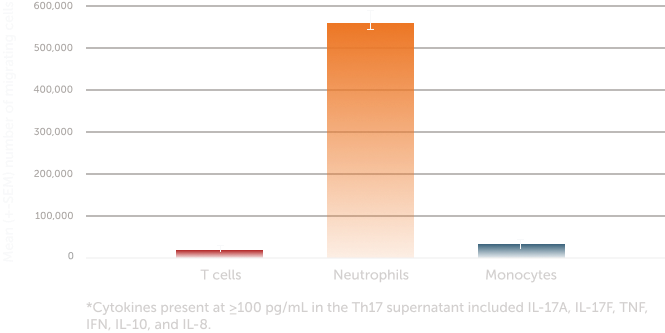
Immune cell migration in response to stimulation with IL-17A and IL-17F was observed in vitro. Following stimulation, migration by T cells and monocytes was observed, but most notable was the increased number of migrating neutrophils.15-17
IL-17 induces neutrophil migration towards the site of inflammation15,16*
Unmet need
The complex pathogenesis of psoriasis materializes in the form of psoriatic plaques, causing clinical symptoms that may severely impact a patient’s quality of life.